ACUTE STROKE
PRE-HOSPITAL EVALUATION:
-
Cincinnati Prehospital Stroke Scale (if
one of these is positive, 72% chance of
stroke)
- Facial Droop
- Arm Drift
- Abnormal Speech
- Inform Hospital
IMMEDIATE ASSESSMENT IN THE ER
- ABCs, Vital Signs. If BP >185/100 give Labetelol 10 mg iv over 2 minutes, may repeat after 10 minutes
- Oxygen if O2 Sat <94
- Glucose
- Stat CT
- Activate Stroke Team
- 12 Lead EKG
- NIH Stroke Scale
This is somewhat counter-intuitive in that a score of 0 means normal! This system measures deficits, not abilities, be aware!
- Is he alert? If he needs minor stimuli to arouse it is 1. If he needs strong stimuli to arouse it is 2. If he wont respond it is 3.
- Does he know the month and his age? If he knows the month OR age, it is 1. If he can't answer either it is 2.
- Can he follow commands? If he can follow only one command it is 1, if he cant follow two commands it is 2
- Does he have a visual field deficit? Extinction on dual stimulation is 1, Hemianopsia is 2, Double Hemianopsia is 3
- Can he move his eye sideways? Gaze preference or Ocular nerve paresis is 1 , Forced deviation is 2
- How is his ability to comprehend and express himself?
- Is is his speech dysarthric? Mild is 1 Severe is 2
- Does he have a facial droop? Flat nasolabial fold is 1, droopy lower face is 2, droopy half face is 3
- Any weakness in his right arm? Drift is 1, If he can move against gravity it is 2, If he can only move with gravity eliminated it is 3, No movement is 4
- Any weakness in his left arm?
- Any weakness in his right leg?
- Any weakness in his left leg?
- Any sensory loss when comparing right and left? mild loss is 1, severe loss is 2
- Any ataxia? One limb ataxia is 1, Two limb ataxia is 2.
- Inattention? Lack of attention on one side is 1. Profound neglect is 2.
INCLUSION CRITERIA FOR TPA
- Above 18
- Ischemic stroke
- Informed consent from patient or family ( 5.8% patients will bleed intracranially, out of which 45% will die)
EXCLUSIONS FOR IV TPA 0-3 HOURS FROM TIME OF ONSET
-
Symptom based exclusions:
- Rapidly improving
- Symptoms of Subarachnoid Hemorrhage (ie, worst headache of one's life)
- Seizure at onset of stroke
-
Physical Exam Based Exclusions:
- SBP >185 or DBP >110
-
Present and Past History based
exclusions:
- Stroke, Head trauma or Brain Surgery within 3 month
- Active Internal Bleeding
- ANY History of ICH, brain tumor , AVM, Intracranial Aneurysm
- Arterial puncture noncompressive site within 7 days
- Lumbar Puncture within 7 days
- Recent pericarditis
-
Lab Based Exclusions:
- Platelet <100,000
- Heparin within 2 days with PTT >1.5 times normal
- Coumadin with INR >1.7 or PT >15
- Known bleeding diathesis
- Glucose <50mg/dl or >400mg/dl
- Current use of direct thrombin inhibitors or direct factor Xa inhibitors with elevated aPTT, INR, platelet count, ECT, TT, or Xa activity assays
-
Radiological Exclusions:
- CT shows intracranial bleeding
- CT shows hypodensity affecting >1/3 of cerebral hemisphere
-
Relative Contraindications:
- GI /GU bleeding within 3 weeks
- Major surgery within 2 wks
- Acute MI within 3 months
- Pregnancy
- Seizure at time of onset of stroke (Because it could be Todds paralysis)
- Minor Symptoms
EXTRA EXCUSIONS FOR IV TPA 3-4.5 HOURS
- >80 yr of age
- Hx BOTH diabetes and stroke
- Coumadin REGARDLESS of INR
- NIHSS >25
- Stroke >1/3 of MCA territory
POST TPA CARE:
- Vitals every 15 minutes for one hour, then every 30 minutes for 6 hours and then every hour until 24 hours are up.
- Severe headache or changes in neuro status is an indication for a stat CT brain
- Do not give any antiplatelet agents or anticoagulants for 24 hours.
- Repeat CT brain at 24 hours to check for any hemorrhagic complications
-
If any hemorrhagic complications are
present:
- 6 units FFP
- 6 units Platelets
- If Fibrinogen <100, Cryoprecipitate 0.15 units / kg IV, repeat Fibrinogen in one hour
- Watch for Angioedema from TPA, treat aggressively
- Blood Pressure Management in s/p TPA patients:
-
If SBP 180-230 or DBP 105-120 :
- Labetelol 10 mg IV over 2 minutes, May repeat in 10 minutes at double the dose. Max cumulative dose in 24 hours is 300 mg
- Do not use Labetelol if 2nd degree block , CHF, cardiogenic shock , HR < 60 or severe asthma.
- Alternative: Enalapril 1.25 mg IV over 5 minutes. May repeat Q6H prn. (In elderly use 0.625mg instead)
-
If SBP >230 or DBP 121-140:
Nicardipine 5mg/hour infusion. Increase by 2.5 mg h increments at 15 minute intervals. Maximum rate 15 mg/hour
-
If DBP >140:
Sodium Nitroprusside 0.5 microgram/kg/minute titrate upto max 5 microgram/kg/minute.
Hold antihypertensives if SBP <140 or DBP <80 .Hold Betablockers if HR <60
Read Other Topics
Read All Pages
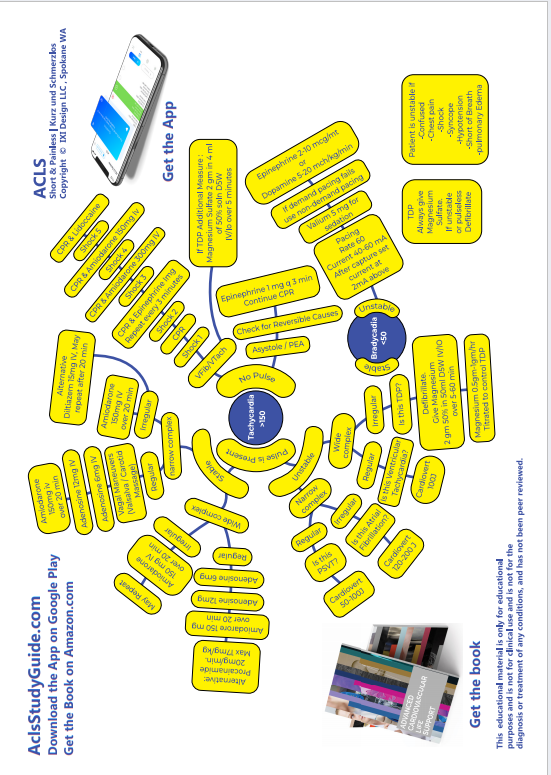
Ventricular Fibrillation
It this was an unwitnessed arrest, meaning it did not happen in front of you, you should give him 5 cycles of CPR...
Read More
Infant Cpr
Perform 30 chest compressions. Use two fingers and deliver the compressions over the breastbone, just below the nipple line...
Read More